INTRODUCTION
The aim of this current study was to assess if Osteopathic Manual Treatment (OMT) has an effect on babies’ colic, considering the change of all the variables of behaviour in a day (sleeping, awake & content, feeding, fussy, crying and unsoothable crying). Moreover not only cranial as in the UK pilot study, but an osteopathic treatment on the entire body was tested.
METHODOLOGY
Participants
The present study, a clinical trial, compared the effects of a phytotherapic product alone with the effect of phytotherapy combined with OMT. 10 participants were recruited through local paediatricians. Treatments were performed by the same osteopath. The research protocol was approved by the BCOM Ethics Committee (Appendix I).
To participate in the study, infants needed to fulfil certain inclusion criteria (Table 1) that feature the colic period [1] and be healthy babies [14]: aged between 2 weeks and 3 months of life, gestational age between 37 and 42 weeks, birth weight between 2.5 and 4 kg, an Apgar index more or equal to 7. Mothers and babies had to be healthy during pregnancy, birth and until the beginning of the study (a part from colic). No limits were put in relation to type of delivery, as others have shown it has no influence on colic trend [15]. Furthermore babies needed to be exclusively breastfed and mothers were requested not to alter their diet during the study period [16-18].
|
INCLUSION |
EXCLUSION |
|
|
AGE |
3 weeks-3 months |
<3 weeks >3 months |
|
GESTATIONAL AGE |
37-42 weeks |
Pre-terms and post-terms |
|
BIRTH WEIGHT |
2.5-4 kg |
<2.5 kg >4 kg |
|
APGAR |
≥7 |
<7 |
|
PREGNANCY |
Healthy |
Complicated or Pathological |
|
BIRTH |
Healthy |
Complicated or Pathological |
|
LIFE |
Healthy a part for colic |
Pathologies |
|
BABY’S FEEDING |
Exclusively breastfeeding |
Bottle or mixed feeding |
|
MOTHER’S FEEDING |
No changes in the diet during the study |
Change in the diet during the study |
|
TREATMENT |
No previous manual Treatment |
Previous manual treatment |
|
Table 1: inclusion and exclusion criteria |
||
Methods
Infants were selected from paediatricians and were diagnosed with colic by means of the Crying Pattern Questionnaire [19-20] (Appendix II).
A written basic explanation of aims, procedure and possible risks of the project were given to the parents/guardians by way of Information (Appendix III) and Risk Assessment Sheets (Appendix IV). Parents were required to consent to take part in the study, after reading these documents by signing the written Consent Form (Appendix V). The babies’ eligibility was confirmed by the Questionnaire (Appendix VI) completed by the parents/guardian about their babies medical history.
During the study the parents were asked to record in a validated Daily Diary [21-22] (Appendix VII) the baby’s behaviour in terms of hours/24 spent sleeping, crying, fussing, feeding and awaking. Details of how to record types of behaviour were explained in the Instruction Sheet (Appendix VIII).
Procedure and Ethical Issues
Babies recruited needed to cry at least 3 hours/day, as mean of the data recorded in the diary during the first 3 days of the study.
Because of the age of the babies some precautions were taken to protect them: a sham treatment was avoided and every infant received with no interruptions at least a treatment having the possibility to try both medical and osteopathic treatment. All data was kept anonymous in the study.
Infants initially attended the control group for 2 weeks, during which they were treated by a standard medical treatment (SMT); it consisted of a phytotherapic product used following the paediatrician’s instruction explained in the Standard Medical Treatment Sheet (Appendix IX). During the 2nd week of SMT, the parents completed the diary, from which babies who cried more than 3 hours per day (as mean of the data recorded) took part in the treatment group. The phase consisted of 3 treatments, a treatment each week for 3 weeks, that lasted about 30 minutes and consisted of gentle cranial and fascial techniques. During the OMT period, manual treatments remained coupled with SMT. During the 3rd week of OMT+SMT parents completed the diary.
Osteopathic Manual Treatment
Treatments were based on the concept of the black box: not a single technique or a standard treatment for every patient, but the approach of every single dysfunction found in the individual patient. In particular, the anatomic regions analysed were:
- JUGULAR FORAMEN: this foramen is the vagus nerve exit that carries to the brain the 95% of gastrointestinal tract afferent messages. Occipital or temporal dysfunctions can distort the jugular foramen, with possible consequences on vagal function [23]. Infants born through a natural delivery showed different cranic base dysfunctions [24].
- DORSO-LUMBAR SPINE: this is the metameric level of the bowel ortosympathetic innervation. Somatic dysfunctions at this level may interact with afferent and efferent signals improving the pain sensation, deteriorating the bowel activity [25].
- UPPER CERVICAL SPINE: vagus and trigeminal nerve are in communication through the spinal trigeminal nucleus. A recent study showed that repeated low intensity stimulus on the vagus nerve gives further stimulus to the trigeminal nucleus, inhibiting it [26]. Somatic dysfunctions of the first cervical vertebrae (where trigeminal nucleus is located) may interact with vagus afferent signals and lead to a distorted message to the vagal nucleus responsible of gastrointestinal tract innervation.
- DIAPHRAGM: one of the possible causes of colic is excess gas in the bowel, which may increase abdominal pressure [1]. Moreover the increased pressure may prevent gas ejection. Osteopathic research has shown that treating the diaphragm may modify intra-thoracic and intra-abdominal pressure [27]. The treatment covered also the other diaphragms (cranic and pelvic, superior thoracic aperture) with which the thoracic diaphragm should harmoniously work [28].
- DIGASTRIC AND SWALLOWING MUSCLES: a hypothesis about pain aetiology during baby’s feeding concerns the spasm of the swallowing muscles [29]. These muscles provoke pain only in the first weeks of life probably because later, getting stronger, the risk of spasm is reduced as in an athlete the muscle strengthening delay soreness onset [30]. The inhibition of digastric and supra-hyoid muscles or the correction of hyoid bone dysfunction may reduce this pain.
Statistical analysis
The endpoints of the study were the parameters recorded in the diary: the mean number of hours/24 in each week of the study spent in sleeping, awake & content, fussing, crying, unsoothable crying and feeding. For each infant the difference of the mean (table 2) of these parameters were valuated from time 0 (T0) to time 1 (T1), from T1 to time 2 (T2) and from T0 to T2. T0 was the time before the beginning of the study, during which babies received no treatments. T1 was the second week of the study, during which infants were treated with SMT, a week after the use of phytotherapic product. T2 was the fifth week of the study, during which babies were treated with OMT+SMT, after the third manipulative treatment. Then the mean difference was tested for significance with repeated measures one way ANOVA for each variable. When test for normality (Shapiro wilk) failed ANOVA on ranks was performed. The software used was SigmaPlot (version 11), post hoc analysis was performed through the Tukey test. P<0.05 was considered statistically significant.
|
SLEEPING |
AWAKE & CONTENT |
FEEDING |
FUSSY |
CRYING |
UNSOOTHABLE CRYING |
|
|
T0* |
10.56 |
4.58 |
3.44 |
1.92 |
2.32 |
1.18 |
|
T1* |
10.82 |
4.95 |
3.16 |
1.76 |
2.14 |
1.17 |
|
T2* |
12.47 |
6.71 |
3.04 |
0.75 |
0.83 |
0.19 |
| *Hours/24 | ||||||
|
SD_0 |
0.82 |
1.46 |
0.64 |
0.88 |
0.24 |
0.09 |
|
SD_1 |
1.21 |
1.43 |
0.34 |
0.77 |
0.27 |
0.16 |
|
SD_2 |
1.46 |
1.62 |
0.37 |
0.35 |
0.29 |
0.22 |
|
Table 2: mean hours of each behaviour in the three moments of the study (T) and standard deviation (SD) of each parameter |
||||||
RESULTS
Sleeping pattern
The results about sleeping (Table 3) show that OMT+SMT was effective in increasing rest hours in comparison with SMT alone (p=.005) and with no treatment (p=.001). However, there was no statistical significance between SMT and no treatment (p=.626). The normality test passed (p=0.066).
|
SLEEPING |
|||||
|
Comparison |
Diff of Means |
T |
Unadjusted P |
Critical Level |
Significant? |
|
T2vsT0 |
1.913 |
3.588 |
0.001 |
0.017 |
Yes |
|
T2vsT1 |
1.650 |
3.095 |
0.005 |
0.025 |
Yes |
|
T1vsT0 |
0.263 |
0.493 |
0.626 |
0.050 |
No |
|
Table 3: One way Analysis of Variance, Dependent Variable: Sleeping |
|||||
Awake & content pattern
The results on awake & content (Table 4) show that OMT+SMT was not significantly effective in increasing calm awake hours in comparison with SMT alone (p>.05). SMT had no significant effect in comparison and with no treatment (p>.05). While SMT+OMT was effective in increasing hours of awake and content in comparison with no treatment (p=.030). The normality test failed (p=.009)
AWAKE & CONTENT
|
Comparison |
Diff of Ranks |
q |
P<0.05 |
|
T2vsT0 |
99.000 |
3.556 |
Yes |
|
T2vsT1 |
78.000 |
2.802 |
No |
|
T1vsT0 |
21.000 |
0.754 |
No |
|
Table 4: One way Analysis of Variance on Ranks, Dependent Variable: Awake & content |
|||
Fussy pattern
The results about fussy (Table 5) show that OMT+SMT was effective in decreasing fussy hours in comparison with SMT alone (p<.001), while SMT showed no significant change in comparison with no treatment (p>.05). Moreover SMT+OMT was effective in decreasing fussy hours in comparison with no treatment (p<.001). The normality test failed (p=.000).
|
FUSSY |
|||
|
Comparison |
Diff of Ranks |
q |
P<0.05 |
|
T0vsT2 |
140.500 |
5.047 |
Yes |
|
T0vsT1 |
6.500 |
0.233 |
No |
|
T1vsT2 |
134.000 |
4.813 |
Yes |
|
Table 5: One way Analysis of Variance on Ranks, Dependent Variable: Fussy |
|||
Crying pattern
The results about crying (Table 6) show that OMT+SMT was effective in decreasing wept hours in comparison with SMT alone (p<.001), while SMT alone had no significant effects in comparison with no treatment (p>.05). Then SMT+OMT was effective in decreasing crying hours in comparison with no treatment (p<.001). The normality test failed (p=.001).
|
CRYING |
|||
|
Comparison |
Diff of Ranks |
q |
P<0.05 |
|
T0vsT2 |
178.000 |
6.394 |
Yes |
|
T0vsT1 |
56.000 |
2.012 |
No |
|
T1vsT2 |
122.000 |
4.382 |
Yes |
|
Table 6: One way Analysis of Variance on Ranks, Dependent Variable: Crying |
|||
Unsoothable crying pattern
The results on unsoothable crying (Table 7) show that OMT+SMT was effective in decreasing colic hours in comparison with SMT alone (p<.001), while SMT alone had no significant effects in comparison and with no treatment (p>.05). Furthermore SMT+OMT was effective in decreasing unsoothable crying hours in comparison with no treatment (p<.001). The normality test failed (p=.048).
|
UNSOOTHABLE CRYING |
|||
|
Comparison |
Diff of Ranks |
q |
P<0.05 |
|
T0vsT2 |
152.000 |
5.460 |
Yes |
|
T0vsT1 |
4.000 |
0.144 |
No |
|
T1vsT2 |
148.000 |
5.316 |
Yes |
|
Table 7: One way Analysis of Variance on Ranks, Dependent Variable: Unsoothable crying |
|||
Feeding pattern
The results on feeding are inconclusive, indeed the differences in the median values among the treatment groups are not great enough to exclude the possibility that the difference is due to random sampling variability. There is no statistically significant difference (p = 0.160).
Meaning of results
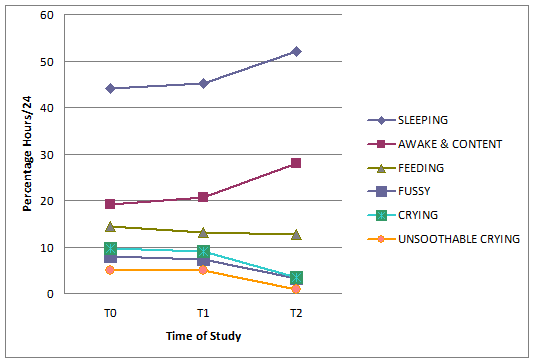
In the 5 weeks of the study infants’ behaviour changed, with an increase in sleeping and awake and content trend, while a decrease in fussy, crying, unsoothable crying trend. Table 8 shows the mean time of hours/24 expressed in percentage at T0, T1, T2. Significant changes appear in unsoothable crying, which trend was about 5% hours/24 both at T0 and T1 was while less than 1% at T2. Similar results emerge from fussy behaviour which trend was more than 7% hours/24 both at T0 and T1 while about 3% at T2. Crying decreases from a trend that was about 9% hours/24 at T0 and T1, to a trend of about 3.5% at T2. Sleeping trend changes from about 44% at T0 to about 45% at T1, to about 52% at T2. Awake and content trend increases from about 19% at T0 to about 21% at T1, to about 28% at T2.
|
% |
SLEE- PING |
AWAKE & CON- TENT |
FEE- DING |
FUSSY |
CRYING |
UNSOOT-HABLE CRYING |
|
T0* |
43.99 |
19.10 |
14.34 |
7.99 |
9.65 |
4.93 |
|
T1* |
45.09 |
20.61 |
13.18 |
7.32 |
8.93 |
4.87 |
|
T2* |
51.96 |
27.98 |
12.65 |
3.14 |
3.47 |
0.80 |
| *% hours/24 | ||||||
|
Table 8: mean percentage of each parameter in the three moments of the study |
||||||
For each parameter there is a greater gap from T1 to T2 than T0 to T1 (graph 1).
Graph 1: percentage hours of each behaviour (sleeping, awake & content, feeding, fussy, crying, unsoothable crying) in the three moments of the study (T0, T1, T2)
DISCUSSION
Comparison of the outcomes
The results of the study show that OMT combined with SMT has an effect in babies with colic in a number of measurable variables.
In the current literature few studies about manipulative treatments on colic symptoms have been performed. Three systematic reviews [8,30-31] and a meta-analysis [9] have pointed out that there is little evidence about the effect of osteopathic treatment in colicky infants’ behaviour.
Nevertheless a UK pilot study has shown an improvement of colic symptoms after cranial osteopathic manipulation [13]. The differences between this and the current study are the variables analysed: the first considered only the parameters of crying and sleeping, while the current considered different types of crying (crying/unsoothable crying) and behaviour, such as fussy, feeding and calm awake. Because of the difference of the variables used, it is difficult to make comparisons between the results of the two studies, although both show significant improvement in the variables measured. The current research has aimed to widen the areas of treatment adding treatment that covers other body areas to the cranial manipulation. This method of evaluation of the entire body was used in a recent exploratory study on preterm infants with changes in gastrointestinal function: it has had positive results in reducing infants’ length of stay in hospital [33]. For this reason it was chosen this approach and not only cranial treatment.
Other studies using manipulative treatment on colicky babies have been done in the chiropractic field [10-12]. Also in these cases some systematic reviews declared the trials analysed small and prone to bias, so not able to give rigorous evidence [8-9,34-35].
However, different clinical trials have had encouraging results: since different medical interventions were studied but no therapy was shown to be completely effective [7-8,36], improvements with a non harmful treatment [40] can be object of interest in literature. Indeed some studies have shown great changes in infants’ behaviour after spinal manipulation both in the short [10,12] and the long term [37].
The variables evaluated were again not exactly the same as the current study, so it would be not correct compare these trials with the present. Moreover in these studies there is no explanation about the techniques used or the dysfunction treated, so it is not possible to compare between the chiropractic and osteopathic approaches.
Limitations of the study
The greatest limitation of the study is the small sample analysed. Although the power of the performed test was 0.886 with α=0.050, thus the sample appears adequate, a wider sample would have allowed to divide the group of treatment from the group of control. The small sample available was linked both to the very strict inclusion/exclusion criteria and the limited length of the enrolment period. The eligibility parameters were chosen on the basis of multiple studies that recognised various elements which may influence colic [8,16-18,38]. Excluding what can modify the phenomenon, there is less influence of other elements on the treatments adopted (OMT and SMT). But this narrowness excluded a lot of possible participants. But the availability of more recruitment time (in the current study it lasted 4 months) would have allowed a more robust project with adequate participants.
A further limitation of the current research is the length of the study (5 weeks) in comparison with the colic period (on average 12 weeks [1]). This aspect was related to the small sample again: clustering the groups of control and treatment the operator could involve double participants. With a wider sample a group could have received before SMT and then OMT and the other group the contrary. Or better each group could have received only one kind of treatment. It would be better because from a statistical point of view the maintenance of SMT during OMT creates not clear results (dragging effect). Moreover SMT may have needed more time to be effective, so it should be left at least the same time to act both for OMT and SMT to do an unbiased comparison (but the time of SMT was reduced to shorten the length of the study).
The choice of proposing both treatments was done for an ethical reason: OMT, is currently not recognised in Italy as a medical intervention, and therefore needed to be offered with a SMT.
To reduce the effect that the time has spontaneously on colic, infants were recruited as soon as possible. The mean age at the beginning of the study was 22.5 days therefore the study was completed when babies were less than 2 months old, age during which colic is normally present.
The last limit of the study was a difficult expressed by mothers to complete such rigorously and for so many days the diary. Although the diary used was validated [19,21,39], the variables analysed are based on people’s perception. It cannot be perfectly objective during a study, even more if people are no blind as in the current study.
Proposal for a larger study
The current research can be considered a pilot study for a next project that could have some different features: a wider sample and the separation of control and treatment groups.
To reduce the length of the study the frequency of OMT can be shortened, e.g. 1 treatment every 5 days. Indeed no adverse effect was recounted by parents and also in wider studies OMT was shown to have no contra-indications [40]. Keeping the preventive measures adopted (Appendix IV) it would be possible to bring the treatments closer to each other.
Eventually for the best clinical result OMT joined with a phytotherapic product may be added to other measures shown to have a role in relieving colic too [7-8,41].
CONCLUSION
The current study has shown that OMT combined with the use of a phytotherapic product appears to improve colic symptoms. In particular it has a role in reducing hours/24 spent in fussy, crying and unsoothable crying, moreover in increasing sleeping and awake & content time. A larger study is requested to make results more significant.
ACKNOWLEDGMENT
I would like to thank my supervisor Dr Patricia Burton for her support in projecting and completing the study and Dr Kerstin Rolfe for her precious advices about the statistical analysis.
I would like to thank Dr Alberto Maggiani who taught my what means doing research for his support in the first part of literature research.
I would like to thank all my teachers for their patient and passion in giving me their experience and for allowing me to end my studies in AIMO.
I would like to thank my parents without whom I would never have become an osteopath.
BIBLIOGRAPHIC REFERENCES
- Illingworth RS, (1954) Three months colic, Arch Dis Child; 29(145):165-74
- Reijneveld SA, Brugman E, Hirasing RA, (2001) Excessive infant crying: the impact of varying definitions, Pediatrics; 108(4):893-7
- Lucassen PL, Assendelft WJ, van Eijk JT, Gubbels JW, Douwes AC, van Geldrop WJ, (2001) Systemathic Review of occurrence of infantile colic in the community, Arch Dis Child; 84:398-403
- Roberts DM, Ostapchuk M, O’Brien JG, (2004) Infantile colic, Am Fam Physician; 70(4):735-40
- Illingworth R.S., (1985) Infantile colic revisited, Arch Dis Child: 60:981-985
- Miller-Loncar C, Bigsby R, High P, Wallach M, Lester B, (2004) Infant colic and feeding difficulties, Arch Dis Child; 89(10):908-12
- Joanna Briggs Institute, (2008) The effectiveness of interventions for infant colic, Aust Nurs J; 16(4):31-4
- Lucassen P, (2010) Colic in infants, Clin Evid; (Online)
- Dobson D, Lucassen PL, Miller JJ, Vlieger AM, Prescott P, Lewith G, (2012) Manipulative therapies for infantile colic, Cochrane Database Syst Rev; 12:CD004796
- Wiberg J.M.M, Nordsteen J, Nilsson N, (1999) The Short-term Effect of Spinal Manipulation in the Treatment of Infantile Colic: a Randomized Controlled Clinical Trial with a Blinded Observer, J Manipulative Physiol Ther; 22(8):517-22
- Olafsdottir E, Forshei S, Fluge G, Markestad T, (2001) Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation, Arch Dis Child; 84(2):138-41
- Miller JE, Newell D, Bolton JE, (2012) Efficacy of chiropractic manual therapy on infant colic: a pragmatic single-blind, randomized controlled trial, J Manipulative Physiol Ther; 35(8):600-7
- Hayden C, Mullinger B, (2006) A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic, Complement Ther Clin Pract; 12(2):83-90
- Silver HK, Kempe CH, Bruyn HB, Fulginiti VA, (1987) Handbook of pediatrics, (eds Appleton & Lange). Norwalk: Conn
- Høgdall CK, Vestermark V, Birch M, Plenov G, Toftager-Larsen K, (1991) The significance of pregnancy, delivery and postpartum factors for the development of infantile colic, J Perinat Med; 19(4):251-7
- Wade S, Kilgour T, (2001) Extracts from “clinical evidence”: Infantile colic, BMJ; 323(7310):437-40
- Hill D.J, Roy N, Heine R.G, Hosking C.S, Francis D.E, Brown J, Speirs B, Sadowsky j, Carlin J.B, (2005) Effect of a low allergen maternal diet on colic among breastfeed infants: a randomised controlled trial, Pediatrics; 116(5):709-15
- Critch JN, Canadian Paediatric Society, Nutrition and Gastroenterology Committee, (2011) Infantile colic: Is there a role for dietary interventions?, Paediatr Child Health; 16(1):47-49
- St James-Roberts I, Conroy S, Wilsher K, (1996) Bases for maternal perceptions of infant crying and colic behaviour, Arch Dis Child; 75(5):375-84
- St James-Roberts I, Halil T, (1993) Infant crying patterns in the first year: normal community and clinical findings, J. Child Psychol psychiatry; 32(6):951-68
- Barr RG, Kramer M.S, Boisjoly C, McVey-White L, Pless I.B, (1988) Parental diary of infant cry and fuss behaviour, Arch Dis Child; 63(4):380-7
- St James-Roberts I, Goodwin J, Peter B, Adams D, Hunt S, (2003) Individual Differences in responsivity to a neurobehavioural examination predict crying patterns of 1-week-old infants at home, Dev Med Child Neurol; 45(6):400-7
- Magoun HI. (2008) Neonati e bambini. In: Osteopatia in ambito craniale, (eds. Futura Publishing Society) pp. 257-287
- Robbins KT, Fenton R.S, (1980) Jugular foramen Syndrome, J Otolaryngol; 9(6):505-16
- Pickar JG, (2002) Neurophysiological effects of spinal manipulation, Spine J; 2(5):357-371
- Lyubashina OA, Sokolov AY, Panteleev SS, (2012) Vagal afferent modulation of spinal trigeminal neuronal responses to dural electrical stimulation in rats, Neuroscience, [Epub ahead of print]
- da Silva RC, de Sà CC, Pascual-Vaca AO, de Souza Fontes LH, Herbella Fernandes FA, Dib RA, Blanco CR, Queiroz RA, Navarro-Rodriguez T, (2012) Increase of lower esophageal sphincter pressure after osteopathic intervention on the diaphragm in patients with gastroesophageal reflux, Dis Esophagus, [Epub ahead of print]
- Nelson KE, Glonek T, (2007) Somatic Dysfunction in Osteopathic Family Medicine. In: Procedures for treating conditions commonly encountered in family practice (Eds Lippincott Williams&Wilkins), pp. 253-254. Crawfordsville: R.R. Donnelley & Sons
- Gudmusson G, (2010) Infantile Colic: Is a pain Syndrome, Med Hypotheses; 75(6):528-529
- Cheung K, Hume P, Maxwell L, (2003) Delayed onset muscle soreness : treatment strategies and performance factors, Sports Med; 33(2):145-64
- Lucassen P, (2007) Infantile colic, Clin Evid (Online)
- Brand PL, Engelbert RH, Helders PJ, Offringa M, (2005) Systematic review of the effects of therapy in infants with the KISS-syndrome (kinetic imbalance due to suboccipital strain), Ned Tijdschr Geneeskd; 149(13):703-7
- Pizzolorusso G, Turi P, Barlafante G, Cerritelli F, Renzetti C, Cozzolino V, D’Orazio M, Fusilli P, Carinci F, D’Incecco C, (2011) Effect of osteopathic manipulative treatment on gastrointestinal function and length of stay of preterm infants: an exploratory study, Chiropr Man Therap; 19(1):15
- Ernst E, (2009) Chiropractic spinal manipulation for infant colic: a systematic review of randomised clinical trials, Int J Clin Pract; 63(9):1351-3
- Ernst E, Canter PH, (2006) A systematic review of systematic reviews of spinal manipulation, J R Soc Med; 99(4):192-6
- Garrison MM, Christakis DA, (2000) A systematic review of treatments for infant colic, Pediatrics; 106(1 Pt 2):184-90
- Miller JE, Phillips HL, (2009) Long-term effects of infant colic: a survey comparison of chiropractic treatment and nontreatment groups, J Manipulative Physiol Ther; 32(8):635-8
- Lucassen PL, Assendelft WJ, Gubbels JW, van Eijk JT, van Geldrop WJ, Neven AK, (1998) Effectiveness of treatments for infantile colic: systematic review, BMJ; 316(7144):1563-9
- St James-Roberts I, Hurry J, Bowyer J, (1993) Objective confirmation of crying durations in infants referred for excessive crying, Arch Dis Child; 68(1):82-4
- Colli R, Biagiotti I, Sterpa A, (2003) Osteopathy in neonatology, Pediatr Med Chir; 25(2):101-5
- Hunziker UA, Barr RG, (1986) Increased carrying reduces infant crying: a randomized controlled trial, Pediatrics; 7(5):641-8